Pant Pant Sigh
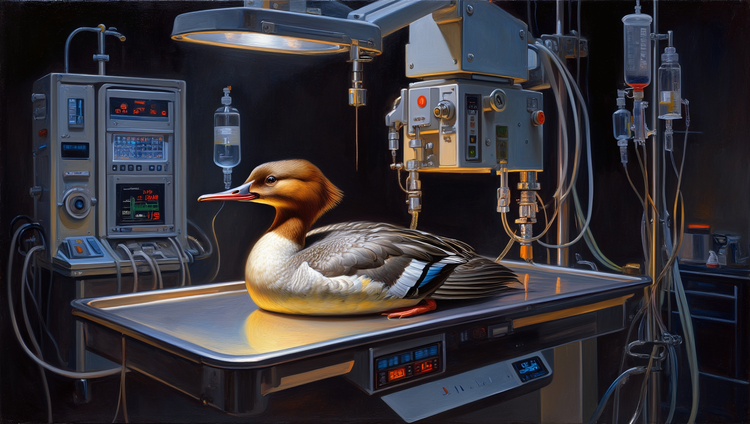
The x-rays were really bad. Much worse than expected. When I had picked Wrigley's chart from the rack of veterinary emergency patients, I have to admit, I wasn't in a huge rush. Although crazy, intense stuff does happen in the ER–most of the time you're just doing ho-hum work, trying to clear the rack and get animals home.
Before I saw the x-rays, I thought I might be able to get him discharged. He was stable and the note from his referral veterinarian had suggested mild pneumonia. They'd seen him earlier in the day, and all I'd seen was "abnormal lungs" in his medical chart. Well, lots of pneumonia cases can be managed as outpatients. He looked stable, and I was just going to double check the radiographs before talking to his owner about my plan.
Okay, he was stressed, but what animal in the ER isn't? Dogs are highly emotional, and the smell of fear and stress and weird cleaning chemicals is enough to–despite our best efforts–turn most of our visitors into complete basket cases. The amygdala, a little almond shaped section of the mammalian brain, is prone to firing off holy crap! signals during emotionally intense scenarios, which lead to automatic physiologic responses. In a scary vet clinic, that often leads to panting.
Owners hate seeing their dogs pant. They've been trained (by TV?) to think their pets will imminently die from thirst as soon as they start panting, and I've waited patiently any number of time while an anxious owner shoves an unwanted water bowl in front of their freaked out animal's face. This kind-hearted action usually has the effect of freaking out the dog even more.
But panting has other causes. It looks like hyperventilation, like the dog has just chased a squirrel across a 12-acre park, but it's a well-regulated system. Oxygen and carbon dioxide stay well balanced during panting. It turns out it's a good way to reduce body temperature, but dogs also pant when stressed, afraid, or in pain. Because panting happens at resonant frequency, it's also low energy. Dogs don't fatigue when panting.
So whatever, Wrigley was panting. Or at least I thought he was. I hadn't gotten a diagnosis from my physical exam,1 so I assumed he was stable. I'd have some time to figure this out with the owner. I'd go chat and get a thorough history. But first I'd review those x-rays.
F—, he's got a pneumo!
Respiratory emergencies really set my amygdala off. I swore in my head (and then out loud, in a childish bid for attention). Pneumos are scary. They kill fast. It's short for pneumothorax: air surrounds and deflates the lung inside the chest (remember sixth-grade biology?). Wrigley had a collapsed lung.
Suddenly, the friendly-but-nervous lab mix in kennel 34 went from an interesting puzzle to a four f–ing alarm fire. He wasn't panting from fear, he was desperately trying to breathe through a lung the size of a chihuahua's. To be clear, he had been struggling to do that at least since those X-rays were taken several hours earlier, but now I was finally aware of it. My advice would be to not work the veterinary ER if you don't like handling hot potatoes.
The good news is that if you're willing to stab you patient in the chest with a large needle, pneumothorax is a very fixable problem. It's seems so wrong, but just get the needle into the pocket of air (i.e. not the lungs or the heart or the aorta) and you can suction it all out, which allows the lung to expand. Problem solved!
I panic-screamed at the nursing staff to get all the crap I needed and meet me at the treatment table ASAFP. Then I panic-called Wrigley's owner and told her to shut up and consent to a thoracocentesis right now so that I could skewer her dog and save it's life.
Wrigley's tongue was now purple (cyanosis from a lack of circulating oxygen). His eyes bulged with existential dread as we pulled him out of his kennel, and he struggled against disorientating injectable sedatives. I took a deep breath as I put on sterile gloves and uncapped a sterile needle thick enough that you could use to sew sailing canvas. The skin of his clipped and scrubbed chest heaved up and down rapidly.
A respiratory crisis is a terrible way to go. Imagine bailing water on a sinking lifeboat, working harder and harder to stay afloat as water creeps up to the railing. The body struggles. It kicks in every mechanism it can think of, but there's no solution for lack of oxygen, animal life's most vital resource.
So I stabbed him in the chest. It's hard not to think of that scene in Pulp Fiction (or The Rock.)2 In reality, it's slightly less dramatic. A big pocket of air in a big dog isn't hard to hit, and pretty soon you and your team (one anesthetist, one person working the syringe, and a couple of looky loos) have made enough space for the lung to fill again.
But Wrigley–half asleep, half panicked–kept on breathing rapidly. Then suddenly that sharp, shallow pattern suddenly changed. His chest stopped moving. We had gotten about a liter of air out of his chest, but were we too late? His heart was still beating, but sometimes it does for a little while, greedily sipping the last molecules of oxygen out of the bloodstream.
We stared at the thick needle still protruding from his chest, waiting for movement. Nothing stirred externally, but there was something happening inside Wrigley. Deep in an ancient network, precious sensory information had been sent and interpreted. It was all done unconsciously. Miraculously, even.
Then Wrigley took the most pleasant, deep and serene breath of his life. A sigh so rich with oxygen and deeply satisfying that it washed away the (physiochemical) panic of one dog and at least four humans away in one blissful instant.
Hey amygdala, you can chill now.
Wrigley was a good patient. He was easy to work with, a huge credit for any non-human species who enters a bizarre structure full of scrubs-wearing primates. Of course, he knew he couldn't breathe, but no veterinary patient ever understands that we're trying to help them. You can be ignorant and still be friendly. His amygdala just wasn't wired for aggression under duress. And I appreciate that.
He went along with it (well, the sedation helped). But he and his amygdala had the wisdom to recognize that panic is all well and good when you're dying, but when the time is right, go slow if you can. Take your time and pull in a patient, double-sized breath. Pop those sweet pulmonary alveoli open to the max.
Breathing is obviously important to stay alive, but it's way more than just a transactional exchange of oxygen and carbon dioxide.3 The breath and the body dance and interact like emotionally-dependent partners, responding to and influencing the expression of joy, pain, worry, anxiety, desire, and relief. To see my patient go from death's edge to restful calm with that spectacular sigh immediately relaxed the urgency of my own autonomic functions.
After Wrigley recovered, I noticed another display of embodied wisdom. This one very dog-specific. As one of the nurses brought him into the lobby to greet his owner, he recognized her. A neurochemical cascade amplified a high salience signal and coordinated a narrow band of muscles on the other end of his body: a hearty tail wag.
- I could have done a better exam and detected absent lung sounds on his left side, but he had been put into an isolation ward and I was using the crappy stethoscope in there and it was loud with beeping and I didn't have anyone to hold him still and a million other lame excuses.
- Those were intracardiac injections, but if I'm stabbing something in the heart things are going significantly worse.
- At its most potent, breathing can induce seizures.




Comments ()